What is the Temporomandibular Joint?
“Consider the joints of the human body. What might first come to mind are the hips and knees—the large joints that support us in our mobility—followed by the wrists, ankles, elbows, fingers, and toes. What can be overlooked, although clearly evident in the mirror, is one of the most used, most necessary, and perhaps most misunderstood set of joints—those of the jaw—which are critical to the vital work of human life, including eating, talking, kissing, and even breathing.” (2020 National Academy of Medicine Report on TMJ)
TMJ stands for Temporomandibular Joint, or jaw joint. The TMJs are the two joints in front of each ear. The joints connect the lower jaw bone (the mandible) to the temporal bones of the skull on each side of the head. The muscles controlling the joints are attached to the mandible and allow the jaw to move in three directions: up and down, side to side, and forward and back. When intact, they are the only joints in the human body that work together as a unit.
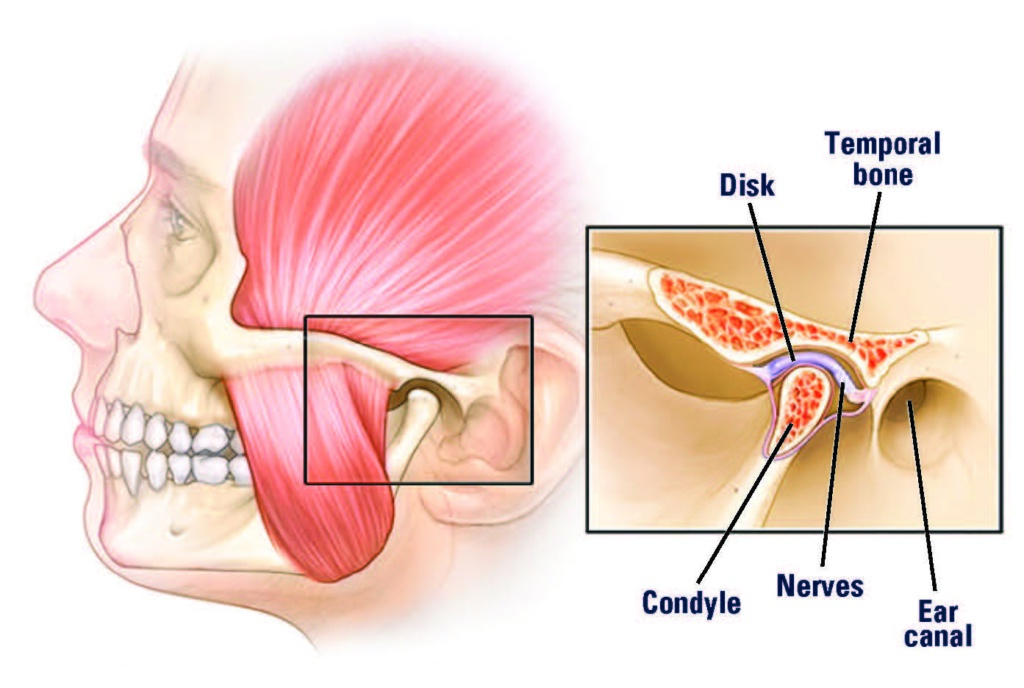
When you open your mouth, the rounded upper ends of the mandible on each side of the jaw (the condyles) glide along the joint socket at the base of the skull. They slide back to their original position when you close your mouth. To keep this motion working smoothly, a soft tissue disc lies between the condyle and the socket. The disc absorbs the shock to the joint from chewing and other movements.
The combination of synchronized, as well as three-dimensional movements of the TMJ, distinguishes the TMJ as the most complicated joint in the body. The TMJ also differs in biological composition from other weight-bearing joints, like the hip or knee.
Jump to a Section Below
What are Temporomandibular Disorders?
Temporomandibular disorders, also commonly referred to as TMJ or TMD, are a complex, under-researched, and poorly understood set of conditions characterized by pain in the jaw joint and surrounding tissues frequently associated with limitation in jaw movements. Recent findings show that TMJ is a complex multi-systems condition involving the circulatory, digestive, endocrine, exocrine, immune, muscular, nervous, reproductive, respiratory, and the skeletal system. TMJ is no longer seen as a condition confined solely to the areas of the jaws and teeth.
Scientists have found that 85% of patients with TMJ also suffer from other conditions – pain and non-pain conditions in other parts of the body. These conditions include allergies, chronic fatigue syndrome, chronic headache, endometriosis, fibromyalgia, interstitial cystitis, irritable bowel syndrome, neck and low back pain, sleep disorders, and vulvodynia.
In addition, connective tissue disorders and autoimmune diseases that can affect the TMJs include: rheumatoid arthritis, juvenile rheumatoid arthritis, juvenile idiopathic condylar resorption, psoriatic arthritis, ankylosing spondylitis, Sjogren’s syndrome, systemic lupus erythema, scleroderma, mixed connective tissue disease, etc. As a result, multiple systems are usually involved.
These other conditions are considered to be comorbid with TMJ because they occur together more often than by chance. In addition, the conditions share other features. These findings are stimulating research into common mechanisms underlying all of these comorbid conditions. Note that many of the comorbidities mentioned are more prevalent or occur exclusively in women.
The left, right or both components of the temporomandibular joint may be involved and, depending on the severity, can affect a person’s ability to speak, chew, swallow, make facial expressions, and even breathe. Jaw muscle disorders are also included as these may accompany jaw joint problems or occur independently.
Who is Affected?
The national prevalence of Temporomandibular Disorders is difficult to estimate due to challenges in collecting data, however estimates range from 10 to over 35 million people in the United States are affected by TMJ at any given time. Clearly, research to understand the prevalence of this condition desperately is needed.
While both men and women experience these disorders, the majority experiencing the most severe symptoms are women in their childbearing years. The ratio of women to men increases with the severity of symptoms, approaching nine women for every one man with major limitations in jaw movements and chronic, unrelenting pain.
What Causes TMJ Disorders?
Adding to the complexity of TMJ disorders is that there are multiple causes, including cases where no obvious cause can be found. Some known causes are the following:
- autoimmune diseases (in which the body’s immune cells attack healthy tissue)
- infections
- injuries to the jaw area
- dental procedures (even prolonged mouth opening during dental treatment)
- overextending the jaw when insertion a breathing tube before surgery
- medication side effects that increase bruxism, exacerbate jaw pain, or cause severe jaw damage (e.g. SSRIs used to treat anxiety, OCD, depression and panic disorders, Antipsychotics, ADHD and Parkinson’s Disease medications, and osteoporosis/bisphosphonate drugs)
- various forms of arthritis
Additionally, there are genetic, hormonal, and environmental factors that can increase the risk for TMJ. Studies have shown that genetic factors contribute to TMJ and are leading to the discovery of new ways of treating TMJ.
The observation that jaw problems are commonly found in women in the childbearing years has also led to research to determine the role of female sex hormones, particularly estrogen, in TMJ.
Symptoms
Symptoms can range from sounds in the joint to severe, debilitating pain and dysfunction. However, some people report no pain but still have problems moving their jaws. Symptoms may include the following:
- pain in the jaw muscles
- pain in the neck and shoulders
- chronic headaches
- jaw muscle stiffness
- limited movement or locking of the jaw
- ear pain, pressure, fullness, ringing in the ears (tinnitus)
- grating in the jaw joint when opening or closing the mouth
- a bite that feels “off”
- dizziness
- vision problems
Keep in mind that occasional clicking or discomfort in the jaw joint or chewing muscles is common and is not always a cause for concern. Often, the problem goes away on its own in several weeks to months.
Diagnosis
The patient’s medical history should not be restricted to the dentition (the teeth and their arrangement) or to the head and neck, but instead a far more comprehensive medical assessment of the patient is needed, which may reveal one or more of the comorbid conditions found to occur frequently in TMJ patients.
The OPPERA study found TMJ disorders are a widespread pain manifested outside the orofacial region with the presence of multiple comorbid persistent disorders in many patients. The most influential predictors of clinical TMJ are simple 20-checklists of comorbid health conditions and nonpainful orofacial symptoms.
Blood tests are sometimes recommended to rule out possible medical conditions as a cause of the problem which may mimic TMJ symptoms. Read more about this topic.
Comorbidities
Scientists have found that 85% of patients with TMJ disorder also suffer from both chronic pain and non-pain conditions in other parts of the body. These conditions are called “comorbid” because they occur together more often than chance can explain. In addition, the conditions share other features, such as similar risk factors, symptoms and underlying disease mechanisms.
These findings are stimulating research into common mechanisms underlying all of these comorbid conditions. Indeed, research indicates that TMJ disorders are a set of complex diseases like hypertension or diabetes involving genetic, environmental, behavioral, and sex-related factors.
Studies have shown that the following 30 health conditions can coexist with TMJ disorders.
- Ankylosing spondylitis in other body joints
- Asthma
- Back, neck, and joint pain
- Chronic fatigue syndrome
- Ehlers-Danlos syndrome
- Endometriosis
- Fibromyalgia
- Irritable bowel syndrome
- Headaches
- Heart disease
- Hypertension
- Interstitial cystitis/painful bladder syndrome
- Juvenile idiopathic arthritis in other body joints
- Neural/sensory conditions
- Osteoarthritis in other body joints
- Poor nutrition due to alerted jaw function and/or pain while chewing
- Psoriatic arthritis in other body joints
- Respiratory conditions (e.g., sinus trouble, allergies or hives, asthma, tuberculosis, breathing difficulties)
- Rheumatoid arthritis in other body joints
- Sinusitis
- Sjogren’s syndrome
- Sleep disorders (e.g., insomnia, poor sleep quality, longer sleep latency, lower sleep efficiency)
- Somatic and psychological symptoms (e.g., depression, anxiety and post-traumatic stress disorder)
- Systemic lupus erythematosus
- Tinnitus
- Vertigo
- Vulvodynia
Not everyone who develops one of these conditions will go on to develop more, however many people with TMJ disorders do, particularly women. Read more about this topic.
Treatments
Most people with TMJ problems have relatively mild or periodic symptoms which may improve on their own within weeks or months with simple home therapy. Self-care practices, such as eating soft foods, applying ice or moist heat, and avoiding extreme jaw movements (such as wide yawning, loud singing, and gum chewing) are helpful in easing symptoms.
According to the National Institutes of Health, it strongly recommends using the most conservative, reversible treatments possible. Conservative treatments do not invade the tissues of the face, jaw, or joint, or involve surgery. Reversible treatments do not cause permanent changes in the structure or position of the jaw or teeth. If TMJ issues become persistent and severe, moving toward aggressive treatments does not necessarily ensure improvement of the symptoms.
Clearly, more research is needed that will lead to the understanding of the condition and development of safe and effective TMJ treatments. As science learns more about the TMJ and its associated structures, many in the health care community are reassessing TMJ treatments and ways in which they were developed. Clearly, the various TMJ disorders are far more complex than previously believed. Read more about this topic.
Insurance Coverage
There are no standardized costs for TMJ treatments. Costs can vary from provider to provider and from state to state. Treatment costs can range from several hundred dollars up to hundreds of thousands of dollars.
Many medical and dental insurance plans do not cover TMJ treatments or only pay for some procedures. Until there are scientifically validated, safe and effective treatments, insurance companies will not pay for treatments that have questionable outcomes. In some situations, your insurance company will not cover costs because TMJ is classified by many insurance companies as a dental and not a medical condition. Contact your insurance company to see if they will cover the cost of a treatment being recommended to you. Read more about this topic.
Who Treats TMJ Disorders?
Since 1936 TMJ has been primarily treated by dentists, however today, we know TMJ to be a complex condition with many biological systems (circulatory, digestive, endocrine, exocrine, immune, muscular, nervous, reproductive, respiratory, and skeletal) playing a role, indicating the need to bring the medical and other allied health professionals in research and patient care.
It’s important to first rule out other conditions that may mimic TMJ symptoms by consulting your medical doctor. For example facial pain can be a symptom or a result of conditions, such as:
- sinus or ear infections
- decayed or abscessed teeth
- various types of headache
- facial neuralgia (nerve-related facial pain)
- tumors
- connective tissue disorders such as Ehlers Danlos Syndrome
- Eagles syndrome
- Dystonia
- Lyme Disease
- Scleroderma
There are no formally developed standards of care for TMJ in clinical dentistry or medicine. Although a variety of health care providers advertise themselves as “TMJ specialists,” most of the more than 50 different treatments available today are not based on scientific evidence of safety and efficacy. These doctors practice according to one of many different schools of thought on how to best treat TMJ.
The National Institutes of Health (NIH) advises patients to look for a health care provider who understands musculoskeletal disorders (affecting muscle, bone and joints) and who is trained in treating pain conditions. Pain clinics in hospitals and universities are often a good source of advice, particularly when pain becomes chronic and interferes with daily life.
Complex cases, often marked by chronic and severe pain, jaw dysfunction, comorbid conditions, and diminished quality of life, will likely require a team of doctors from fields such as neurology, rheumatology, pain management, and other specialties for diagnosis and treatment.
Stigma
The lack of credible information relayed to the public and professionals about the reality of impact that TMJ can have on one’s overall health and life results in patients continuing to suffer in silence and isolation because nobody – including family, friends, employers, etc. – can comprehend how multiple therapies, including years of treatments at exorbitant costs cannot fix or alleviate the problem but seem to worsen it. It is always the fault of the patient when things don’t work out like they were told it would, leaving the patient to question what they did wrong.
Advertisements portray TMJ as a simple click and pop that can easily be fixed. TMJ is often trivialized by the dental and medical communities as an insignificant problem.
Adding to the stigma for many TMJ patients, are the physical changes to their face as a result of surgical “readjustments”, paralysis, etc. Many patients express despair that they don’t recognize themselves anymore. Patients have also told us that they are embarrassed to be seen or to eat in public, because chewing and swallowing are difficult, they choke, and/or food falls out of their mouths. Speaking and enunciating words properly is often difficult and also embarrassing. Facial paralysis and the inability to smile is often times misinterpreted as a foul personality. Read more about this topic.
FAQs
We are frequently asked questions. Click here to read more.
